Raising the standards against COVID-19
The global health system is under siege
According to the latest numbers reported on Monday the 11th of March 2020 (link 1), 118,162 cases of COVID-19 have been confirmed and 4,290 people have died across 113 territories, meaning the global mortality rate has risen slightly from previous estimates of around 2% to approximately 3.6%.
It is likely that the global incidence will continue to rise steadily as the capacity and resources to identify potential carriers and diagnose the condition become more widespread and available, even in low-income regions. It is also possible that we will see a plateau in this trend once vaccines and therapies have been developed and are available to the general public. However, there are still many questions to be asked as we learn more about the disease.
Fact over fiction
The most pressing question on the minds of many South Africans is the following: are we, as a nation, ready and able to fight back against this novel adversary?
The field of knowledge surrounding COVID-19 is burgeoning at an impressive rate with multidisciplinary teams from WHO, National Health Authorities, and research institutes collaborating and toiling around the clock to characterise the disease and identify the patterns of transmission in order to develop targeted interventions and halt its spread.
A recent study by Gilbert et al (link 2) analyses the readiness of African states to identify the virus and cope with the possible effects of secondary transmission. The researchers identified countries with the highest risk of importing COVID-19 based on air traffic volume between these regions and Chinese provinces. Countries flagged as danger zones for importation include South Africa, Algeria, and Egypt, with the latter currently leading the continent in terms of number of confirmed infections (link 3).
The study also determined preparedness and vulnerability of local health systems to cope with an outbreak. This was achieved using two robust measurement instruments:
• State Party Self-Assessment Annual Reporting (SPAR) tool—this forms part of the WHO IHR MEF (International Health Regulations Monitoring and Evaluation Framework) and evaluates a country’s functional capacity and ability to respond to health emergencies using 24 indicator scores (for example, laboratory capacity, available human resources, established surveillance measures etc.)
• Infectious Disease Vulnerability Index (IDVI)—this system accounts for non-functional, indirect factors that form part of the wider health system and that may affect a country’s ability to manage epidemics (for example, current socioeconomic and political conditions)
Where does South Africa rank in terms of preparedness?
Although South Africa ranks high in terms of importation risk, the country has a stronger health system in comparison to other high-risk regions such as Nigeria, Kenya, Ghana, and Tanzania which not only experience elevated air traffic volumes with China but also have more vulnerable health systems with fewer resources. In fact, South Africa even performs reasonably well relative to the Organisation for Economic Co-operation Area (OECD) member countries—which are mostly developed nations from Europe—in terms of its SPAR and IDVI scores.
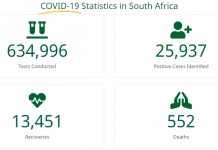
At the beginning of February, South Africa was one of only two African countries with the capabilities to test for COVID-19 (link 4)—there are now over 40 African countries that are able to diagnose patients (link 5)—and health minister Dr. Zweli Mkhize has been at the forefront of updating the nation on new cases and the management of those who have been diagnosed. Communication from Government authorities, most notably the National Institute for Communicable Diseases (NICD), has been commendable in alerting South Africans to new cases and providing practical information to citizens who are worried about the future impact of the disease on everyday life.
A less-obvious danger facing the continent is the precarious position of low-risk importation countries with the weakest health systems, for example, the Democratic Republic of Congo, Mozambique, Senegal, and Cameroon. These nations are at an elevated risk once local cycles of transmission begin to proliferate in other African states, with unregulated cross-border travel posing a new threat. Cases have already been reported in Senegal and Cameroon. Health systems strengthening (HSS) efforts should be focused on these countries, including improving supply chain management practices to ensure the necessary medical resources are available in the areas with greatest need.
Key practices to reinforce health systems and create healthy societies
Sound infection prevention and control (IPC) practices form the backbone of safe, quality healthcare service. This applies to all levels of the health system; from clinic and hospital-based care to community and home-based care. These environments present themselves as high-risk settings as healthcare professionals and non-clinical personnel are exposed to pathogens (such as COVID-19) on a daily basis and, if infected, may catalyse transmission. Furthermore, these settings contain a high concentration of individuals at greatest risk of contracting COVID-19 and succumbing to the disease, i.e., the elderly as well as those patients with compromised immunity and who are already struggling with underlying health conditions.
Indeed, international standards have been set locally to guide service providers to attain optimal levels of performance and to provide a sanitary and safe environment for patients and their families. For example, IPC is covered extensively in the healthcare facility standards set by the Council for Health Service Accreditation of Southern Africa (COHSASA). This element feeds into clinical and non-clinical areas (such as food and laundry services). The overview of the IPC standards states that “the goal of a facility’s infection surveillance, prevention and control system is to identify and reduce the risk of acquiring and/or transmitting infections among patients, personnel, contract workers, volunteers, students and visitors.” Key elements at the forefront of effective risk mitigation strategies entail establishing proactive surveillance systems, compliance with correct handwashing procedures, and appropriate use of personal protective equipment (PPE).
It is also noteworthy that IPC applies to other public areas such as restaurants and shopping malls, and everyone is required to make a concerted effort to promote clean and sanitary public spaces.
Practical steps to promote IPC and prevent transmission
• Don’t stock up on PPE, such as masks, as health workers on the frontline desperately require this equipment in order to protect themselves and their patients
• Wash your hands with soap thoroughly and regularly
• Cough into your arm and sneeze into a tissue
• Avoid unnecessary contact with others (for example, avoid shaking hands)
• Avoid large crowds and public gatherings, i.e., social distancing
• Avoid unnecessary travel to high-risk regions (for example, China, Iran, South Korea, and Italy)
Remaining informed through the correct channels
Pockets of misinformation about COVID-19 have appeared over recent weeks (especially via social media platforms), leading to unnecessary hysteria. Therefore, we must remain cautious when presented with new insights and information. I would recommend visiting the open access Lancet COVID-19 Resource Centre (link 6) and WHO Coronavirus disease (COVID-19) outbreak webpage (link 7) for reliable, factual, and up-to-date developments on the virus.
Links
- https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30411-6/fulltext
- https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd
- https://www.africaportal.org/features/africa-enters-critical-stage-corona-virus-response/
- https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30464-5/fulltext
- https://www.thelancet.com/coronavirus
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019